Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Reductive Factors for Preventing the Development of Caries and Periodontal Diseases in Children with ASD Aged 3 to 18 in Tbilisi
*Corresponding author:Maka Sabashvili, Associate Professor of School of Health Sciences, Dentistry Department, The University of Georgia,Tbilisi, Georgia.
Received:March 08, 2023; Published:March 30, 2023
DOI: 10.34297/AJBSR.2023.18.002468
Abstract
According to HWO 2013 data, the prevalence of autism was 160:1 (WHO, 2013), and currently this proportion has changed significantly at the expense of increasing the number of patients and ratio is 59:1. Due to the increase in the number of autisms, dental services have also moved forward. Therefore, the reductive factors for preventing the development of caries and periodontal diseases should be determined. 322 patients were examined, age ranged from 3-18 years. 249 male and 73 female were included in the study. The research tool for the analytical component of the study was a questionnaire with 46 questions. Research has shown that to prevent caries and periodontal disease, children with ASD should have preventive visits to dental clinics every 6 months, which can be funded mainly by state insurance, which will have a positive effect on the timely diagnosis of diseases, reducing early extractions and avoiding jaws-system disorders.
Background
The health of teeth and gums is associated with several factors. In the European region, the burden of oral diseases and other chronic diseases can be significantly reduced by correctly and purposefully implemented preventive measures, in the implementation of these measures it is important to identify common risk factors. Wellplanned and implemented preventive interventions and policies are important for increasing quality life-years (QALYs). based on scientific studies, oral health indicators in patients with autism spectrum disorder and their correlation with social conditions of patients with ASD have not been evaluated. Correlation of these data with oral disease (caries-K02, gingivitis and periodontal diseases-K05) and correlation of obtained data with hygiene index. Accordingly, it is not known specifically which risk factors influence the oral health status of dental patients aged 3 to 18 years with ASD, namely the development of caries and periodontal diseases, and preventive measures for oral diseases in patients with autism spectrum disorder have not been developed.
Methods
Our research methodology provided for the study of the main group according to various factors (gender, age, etc.), therefore the number of respondents to be investigated was 322 patients. Age ranged from 3-18 years. Of the individuals included in the study, 249 (77.3%) were male, and 73 (22.7%) were female.
Results
Caries was detected in 65% of the investigated contingent. The presence of concomitant diseases was found to be an important factor in tooth damage. 87.7% of the interviewed children with ASD who had co-morbidities had DMF, and 61.5% of those who did not. Taking medication was also found to be an important factor in the development of caries, in children with ASD, the average DMF index was 8.6 when taking medication, and 5.9 when not taking it. Also, factors which are important to develop caries are foods and oral care.
Conclusions
Reduction factors were identified that would have a positive and/or negative effect on the oral health of the contingent included in our study. It was determined that the spread of oral diseases is facilitated by improper hygienic cleaning at home, the type of food products consumed, the presence of concomitant diseases, the effects of medications taken in the presence of concomitant diseases, and the presence of harmful habits.
Key words:Autism, Oral health, Factors
Introduction
The etiology of autism is multifaceted. There is no specific causative factor. Autism Spectrum Disorder (ASD) is a condition characterized by impaired social communication as well as restricted and repetitive behaviors. It is considered a neurodevelopmental disorder because it is associated with neurological changes that may begin prenatally or early postnatally, alter the typical pattern of child development, and produce chronic signs and symptoms that typically appear in early childhood and have potential longterm consequences [1,2]. The oral health care of such patients can be difficult because they cannot analyze any kind of dental problem, in most cases they cannot convey to their parents/guardians what they are worried about, what kind of pain they have, etc. Autistic spectrum patients, as children with special needs, constitute a small percentage of the population and require unique management due to their behavioral characteristics [3,4]. According to literature data, dental diseases are frequent in patients with autism spectrum, in particular - caries, periodontal diseases and, depending on their behavior - self-injuries, both in the oral cavity and outside the mouth. The above-mentioned diseases have a negative impact on the life of both healthy children and children with autism spectrum disorder [5]. As mentioned above, dental problems in children with autism spectrum disorder are difficult to manage, which is reflected in their oral health status. Autistic individuals with higher rates of periodontal problems were found to have lower caries rates. A low caries prevalence was reported in a study by Kamen and Skier [6]. Low and Lindemann evaluated the primary dentition of patients with autism spectrum disorder, examining the DMF index (caries, extracted and impacted teeth). During the initial examination, the DMF index was quite high and was reduced based on followup observations. which was caused by the inclusion of preventive measures and appropriate education of dentists. Autistic children have impaired tongue movement, so they prefer soft foods that they swallow without chewing. Gingival hypertrophy induced by medication was detected in children with ASD. Also, according to studies, it is established that in this population, a high amount of sugar was used. A comparison was made between patients with ASD and patients with typical development, and the proportion of sugar consumption was very high in patients with ASD, which certainly affects the oral status, plaque formation and caries development. The author explains the difference in percentage by the fact that sugar has a calming effect, so parents try to meet the child’s requests for sugary foods, especially when managing a certain situation becomes problematic [7]. Dental injuries are common in autistic spectrum patients, due to the patient’s bad habits, such as biting the nails, biting the lips and cheek mucosa, putting, and sucking foreign objects in the mouth, etc. [8].
Materials and Methods
The research tool for the analytical component of the study was a questionnaire with 46 questions, through which the biological and social factors causing caries were revealed. The said questionnaire was approved by the Bioethics Council, and it fully met the ethical aspects of the research. The used questionnaire included such biological and social factors as: age of recruited children; gender; nationality; demographic data; socio-economic situation; the presence of concomitant diseases; the need for medication; food ration and its diversity; Harmful habits, diagnosis time, sensory problems, peculiarities of behavior with the doctor, peculiarities of oral hygiene habits; type of toothpaste used and frequency of use; determining the type of toothbrush used, the average number of teeth affected by caries; the number of extracted and extracted teeth; Dental visits and treatment methods. Due to objective reasons, the respondents could not fill in the mentioned questionnaire directly, so the questionnaire was filled by the parent and/or guardian of the children/adults. Clinical examination of the oral cavity of patients with ASD was performed using a dental mirror and a probe to detect caries. Also, counting the missing and extracted teeth and calculating the DMF index. Visual examination of the gums and evaluation of the degree of gingivitis was also performed. The incidence of oral diseases has significantly increased in recent decades for all categories of people. To find out the characteristics of the group with ASD, we additionally interviewed children and adolescents with typical development with approximately the same characteristics as the main research group, whose number also amounted to 322 patients. This method allowed us to strictly distinguish the features of oral diseases of the respondents with ASD. Based on the purpose of the research, several centers involved in the habilitation program for children with autism spectrum disorder were selected in Tbilisi, where the examination of children with autism spectrum disorder and the survey of parents/guardians were carried out. Respondents aged 3 to 18, both female and male, were selected. The sample size of the research group is at least 291 pediatric individuals with ASA across Tbilisi. n = N*X / (X+N–1), X = Zα/22*p*(1-p) / MOE2, where Zα/2 is the critical value of the normal distribution at α/2 (when the confidence level is 95%, α is 0.05 and the critical value is 1.96); MOE is the margin of error, p is the sample proportion, and N is the population size.
Results
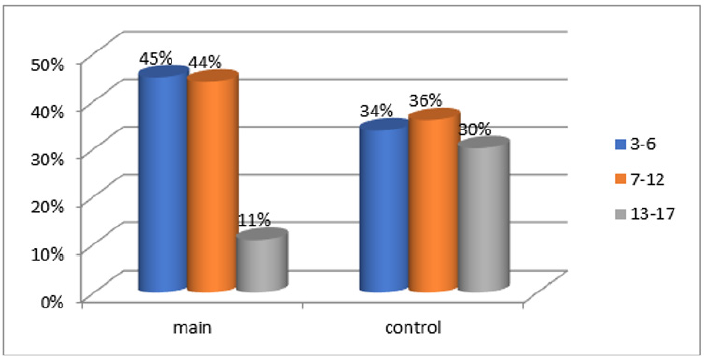
According to the research methodology, 322 patients with ASD, 322 typically developing individuals, 170 pediatric dentists and 53 dental clinic managers were included in the study. 249 of the patients with ASA were male and 73 were female. The research contingent was divided into three age groups: respondents aged 3-6, 7-12, 13-18. The age division was determined by the particularity of dentition, milky, mixed, and permanent dentition period. 45% of all examined patients of the main group were 3 to 6 years old, 44% were 7-12 years old, and 11% were 13 to 18 years old. 34% of respondents aged 3-6 years old, 36% aged 7-12 years old, and 30% aged 13-18 years old of the control group [Figure 1].
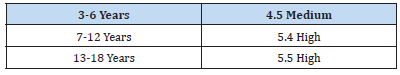
Caries was detected in 65% of the examined contingent, according to age groups it was distributed as follows: 3-6 years - 43%, 7-12 years -67%, 13-18 years -64%. The DMF index of the control group was 3.1, and the prevalence of caries was detected in 33%. Using a questionnaire as a research tool, an in-depth interview of the respondents’ parents/guardians was conducted. As a result, information about co-morbidities of the recruited children was obtained. 11.8% (67 cases) of respondents in the full study group had various chronic diseases or conditions, including allergic reactions. The presence of concomitant diseases was found to be an important factor in tooth damage. Among the identified comorbidities, the types of diseases are different, however, in the presence of comorbidities in children with ASD, the average DMF was equal to 6.0, in the absence - 4.5. The same rate in the control group was 3.5 and 1.8. Which means that the presence of diseases in ASD patients is an additional contributing factor to increase the rate of tooth damage. 87.7% of the interviewed children with ASD who had co-morbidities had DMF, and 61.5% of those who did not. χ²=17.5 and P=0.001, which means that there is a statistically significant relationship between comorbidity and tooth damage. P=0.001 and Cramers=0.165, which means that there is a low but reliable positive correlation between comorbidity and dental disease. In the case of concomitant disease, the chance of tooth damage is 3.13, and in the absence of it is 0.7, OR=4.46. That is, the comorbidity risk factor is important. A two-sided confidence interval of 95% was determined by the Mantel-Haenszel test (OR=4.46; 95% CI 2.1-9.5); The influence of comorbidities in relation to the risk of developing oral cavity pathologies was evaluated by Mentel-Haenszel stratified analysis. According to the obtained data, the risk of developing oral pathologies is 4.4 times higher in subjects who have any chronic or concomitant diseases, compared to those who were practically healthy, without any chronic or concomitant diseases (OR MH=4.4; 95% CI OR MH =2.0-9.5). Those who had co-morbidities needed to take medication. In children with ASD, the average DMF index was 8.6 when taking medication, and 5.9 when not taking it. For the control group receiving 5.3, not receiving 1.6. According to the obtained data, the risk of developing oral pathologies is 10.1 times higher in subjects who used any type of medication compared to those who were practically healthy and did not need to use medication (OR MH=10.1; 95% CI OR MH 5.5-18.4). 84.9% of the examined patients clearly performed routine home hygiene, which was manifested by brushing of their teeth, 36.2% of them brushed occasionally and once a day, and 27.6% brushed twice a day. 41.6% did sometimes by themselves, sometimes with the help of their parents, while 29.5% brushed by themselves, in 26.5% cases oral hygiene was done only with the help of their parents. 8.3% did not use a toothbrush, which was related to their sensory problem, and out of 91.7% who used a brush, 69.3% of them used a manual brush, 22.9% an electric one, 14% both. The frequency of tooth brushing takes one of the leading places in the formation of tooth damage. ASD children who brushed their teeth twice a day had an average of 3.8, those who brushed once a day - 4.3, and those who brushed occasionally 5.1. For the control group, respectively: 0.8- 1.7-4.1 points. As the analysis showed, in both cases, the frequency of scratching affects the DMF coefficient, although it is more noticeable in the control group, because in children with ASD, other factors besides scratching also act at the same time. According to the literature, dietary diversity is closely related to oral health, particularly caries and periodontal diseases. This correlation was also revealed in the results of our research. The effect caused by the food factor is very high. Those whose favorite foods were baked goods, sweets and chips caries prevalence was in 95.7% of those surveyed, and those who ate mostly fruits, vegetables, meat, and dairy products had 58.9 percent. χ²=49.5 and P=0.001, which means that there is a statistical relationship between the type of food and tooth damage. P=0.001 and Cramers=0.392, which means that there is a medium strength positive correlation between food type and disease. In case of eating unhealthy food, the chance of tooth damage is 9.43, and in case of eating healthy food, it is 0.6, OR=15.3. That is, the food risk factor is important. A two-sided confidence interval of 95% was determined by the Mantel-Haenszel test (OR=15.3; 95% CI 6.0-39.1) (Table 1).
Discussion
As a result of the research, we identified the factors affecting the health of the oral cavity and the status of the oral cavity, under the influence of which the risk of spreading caries and periodontal diseases was increased. Reduction factors were identified that would have a positive and/or negative effect on the oral health of the contingent included in our study. It was determined that the spread of oral diseases is facilitated by improper hygienic cleaning at home, the type of food products consumed, the presence of concomitant diseases, the effects of medications taken in the presence of concomitant diseases, and the presence of harmful habits. Also, because dental treatment is considered one of the most expensive treatments in the world, the socioeconomic status of patients with ASD affects oral health, as patients with low social status, along with other factors, do not receive proper dental treatment, which reflects Oral health, and not just oral health, generally affects the general state of human health, which consequently affects the public health burden.
Conclusions
The analysis of the results of the study allows us to make
important conclusions regarding the prevalence of periodontal
diseases and caries in patients with autism spectrum disorders, as
well as the reception of dental services:
a) Due to the influence of various factors (nutrition,
hygiene, concomitant diseases, etc.), the prevalence of caries in
patients with ASD is twice as high as in the case of the control
group. Along with the number, the rate of intensity of caries
significantly prevails (5.1) and becomes severe in patients with
ASD, which often ends with extraction instead of treatment.
b) Dental services are one of the most expensive procedures
compared to other medical services. Consequently, oral health
status in ASD patients with low social status was worse than in
families with moderate and especially high social status.
c) Patients with ASD are often restricted to eating a
homogeneous diet, which is often limited to sweet, baked, and
porous foods, which on the one hand leads to a lack of minerals
and vitamins, on the other hand reduces the mechanical
gingival process and on the other hand promotes the spread of
abnormal bacteria in the mouth. Consequently, unhealthy food
risk factor is high in relation to healthy eating.
d) In patients with ASD, less oral and often inadequate
attention is paid to the oral cavity. This is manifested in the
practice of brushing teeth rarely, or not at all, in the ignorance
of the mouth at least rinsing with water, and so on. Which is why
low oral hygiene was established as a high-risk factor (OR=9.9,
CI=4.5-21.9).
e) Healthy food (fruits, vegetables) (OR=15.3,95% CI=3.9-
22.6) and good oral hygiene in children and adults aged 3 to
18 living in Tbilisi OR=9.9,95% CI=3.1-12.4) are reducing
factors, have a positive effect on oral health and help prevent
the development of periodontal and carious processes.
f) Patients with ASD often have a variety of concomitant
pathological diseases, some of them directly (causes weakening
of the teeth and gums, etc.), and some indirectly (causes a
decrease in saliva secretion, deterioration of saliva quality, etc.)
affect the formation of caries, which included the presence of
concomitant disease in the group of significant risk factors
(OR=4.4, CI=2.09-9.5).
g) The presence of comorbidities and other needs often
requires the use of high-frequency medications. Most of them
directly and often indirectly adversely affect the oral cavity and
lead to the development of periodontal and carious processes.
Accordingly, the impact of medications on oral health is a
negative risk factor (OR=10.1, CI=5.5-18.4).
Declarations
Ethics approval and consent to participate. The questionnaire was approved by the Bioethics committee (11-5308), and it fully met the ethical aspects of the research.
Availability of Data and Materials
Electronic-form transcripts of the conducted interviews and signed consent forms are all in possession of the author. The thesis can be freely accessed, which previously been published in doctoral program of The University of Georgia [9].
Conflict of Interest
The author declares no potential conflicts of interest.
Funding
There were no external funding sources.
Contributions
M.S contributed to the conception and design of the study..
Acknowledgements
We would like to thank Georgia and Tbilisi Autism Rehabilitation Center, children, and their parents for giving us access to conduct this study. We also like to acknowledge the help and contribution of the doctors and other assisting staff of dental clinic “UG DENT”.
References
- Christensen D, Zubler J (2020) CE: From the CDC: Understanding Autism Spectrum Disorder. Am J Nurs 120(10): 30-37.
- Ben Sasson A, Hen L, Fluss R, Cermak SA, Batya Engel Yeger, et al. (2009) A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. J Autism Dev Disord 39(1): 1-11.
- Susan L Neely Barnes, Heather R Hall, Ruth J Roberts, J Carolyn Graff (2011) Parenting a Child With an Autism Spectrum Disorder: Public Perceptions and Parental Conceptualizations, Journal of Family Social Work 14(3): 208-225.
- Colizzi M, Sironi E, Antonini F, Marco Luigi Ciceri, Chiara Bovo, et al. (2020) Psychosocial and Behavioral Impact of COVID-19 in Autism Spectrum Disorder: An Online Parent Survey. Brain Sci 10(6): 341.
- Sheiham A (2006) Dental caries affects body weight, growth and quality of life in pre- school children. J Br Dent 201(10): 625-626.
- Kamen S, Skier J (1985) Dental management of the autistic child. Spec Care Dentist 5(1): 20-23.
- Kuter B, Guler N (2019) Caries experience, oral disorders, oral hygiene practices and socio-demographic characteristics of autistic children. Eur J Paediatr Dent 20(3): 237-241.
- Chandrashekhar S, Jyothi S Bommangoudar (2018) Management of Autistic Patients in Dental Office: A Clinical Update. International Journal of Clinical Pediatric Dentistry 11(3): 219-227.
- https://ug.edu.ge/storage/disertations/February2022/kNCr9jPcliHkzf9XSfMV.pdf.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.